Case Study:You work in a women’s health clinic. Many come lower abdominal discomfort. with Chronic Pelvic Pain (CPP).
Questions to answer
Discuss and described the pathophysiology and symptomology/clinical manifestations.
Give three examples with definition of Chronic Pelvic Pain (CPP) of:
I. Gynecologic origin with ICD 10 numbers.
II. Non-gynecologic origin with ICD 10 numbers.
Discuss patient education.
Develop the management plan (pharmacological and nonpharmacological).
An effective health assessment incorporates not only physiological parameters; please suggest other parameters that should be considered and included on health assessments to reach maximal health potential on individuals.
Name the different family developmental stages and give examples of each one.
Describe family structure and function and the relationship with health care.
Sample Answer
Chronic Pelvic Pain (CPP)
Pathophysiology and Symptomology
Chronic pelvic pain (CPP) is defined as noncyclical pain of at least 6 months' duration that is localized to the pelvis, abdominal wall, or buttocks and is severe enough to cause functional disability or require medical attention.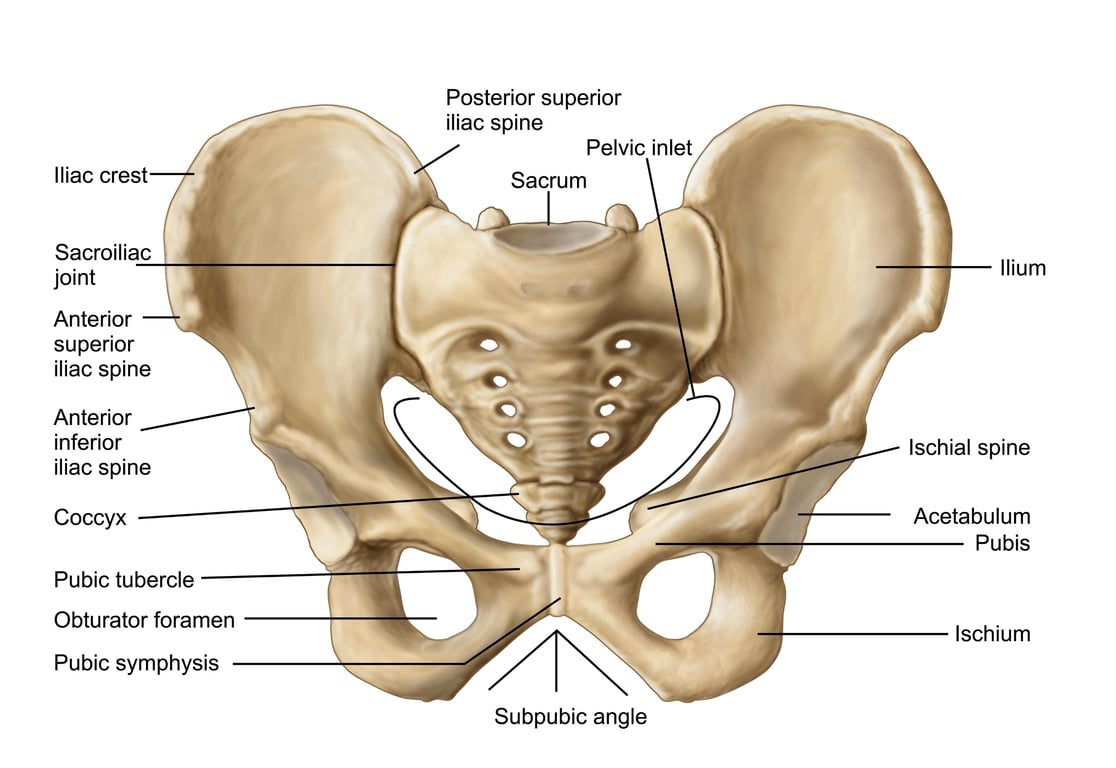 Licensed by Google
Licensed by Google
Its pathophysiology is complex and often multifactorial. It is thought to involve a combination of biological, psychological, and social factors. The pain can originate from a single source, but chronic pain often leads to central sensitization, a state where the nervous system becomes hypersensitive. This means pain signals are amplified, even with minimal stimulation, and can spread to other areas. This is why CPP can persist even after the initial cause is treated.
The symptomology of CPP is highly varied but can include:
Constant or intermittent pain in the lower abdomen or pelvis.
Pain during or after sexual intercourse (dyspareunia).
Pain during urination or bowel movements.
Pain while sitting or standing for long periods.
Referred pain to the lower back, buttocks, or thighs.
Examples of CPP Causes
I. Gynecologic Origin
Endometriosis: A condition where tissue similar to the lining of the uterus grows outside of it. This tissue responds to hormonal changes, causing inflammation, pain, and sometimes scar tissue.
ICD-10 Code: N80.9 (Endometriosis, unspecified).
Pelvic Inflammatory Disease (PID): An infection of the female reproductive organs, often caused by sexually transmitted bacteria. A past or current infection can cause inflammation and scarring, leading to chronic pain.
ICD-10 Code: N73.9 (Female pelvic inflammatory disease, unspecified).
Adhesions: Bands of scar tissue that can form after surgery or infection, causing organs to stick together and restrict movement, leading to chronic pain.
ICD-10 Code: N99.4 (Postprocedural pelvic adhesions).
II. Non-Gynecologic Origin
Interstitial Cystitis/Bladder Pain Syndrome: A chronic bladder condition that causes bladder pressure, bladder pain, and sometimes pelvic pain. The cause is unknown, but it involves a breakdown of the bladder's lining.
ICD-10 Code: N30.10 (Interstitial cystitis without ulceration).
Irritable Bowel Syndrome (IBS): A common disorder affecting the large intestine, leading to cramping, abdominal pain, bloating, gas, and diarrhea or constipation. The pain can be perceived as pelvic pain.
ICD-10 Code: K58.9 (Irritable bowel syndrome without diarrhea).
Pelvic Floor Muscle Dysfunction: Spasms or chronic tension in the muscles of the pelvic floor, which can cause severe pain in the pelvic area and make daily activities difficult.
ICD-10 Code: M62.838 (Other muscle spasm of other specified site).
Patient Education
Patient education is paramount for managing CPP due to its complex nature. The provider should:
Validate the patient's pain: Acknowledge that the pain is real and that they are not imagining it. This builds trust and encourages adherence to the management plan.
Explain the multifactorial nature of CPP: Help the patient understand that the pain may not have a single, simple cause and that a holistic approach is necessary.
Provide a comprehensive overview of the management plan: Explain the purpose of each pharmacological and non-pharmacological treatment.
Set realistic expectations: Emphasize that relief may not be immediate and that finding the right combination of treatments can take time.
Encourage a multidisciplinary approach: Explain the value of working with specialists like physical therapists, pain management physicians, or mental health professionals.